Rhizarthrosis is defined as degeneration of the trapezium-metacarpal joint, characterised by abrasion, the progressive deterioration of the joint surfaces and newly-formed bone in the joint.

The significance of this pathology lies in the functional impairment it causes, and the frequency with which it occurs. The thumb accounts for 40% of hand function, and the trapeziometacarpal joint is the most important part of its osteoarticular structure. The biomechanics of the joint structure allow for the formation of a clip between the thumb and the middle fingers, and the creation of a strong grip. It is therefore clear that the functional importance of this joint explains the fact that any pathological process that alters it could lead to chronic social and occupational disability and have significant repercussions on everyday activities.
The trapeziometacarpal joint is also one of the most common sites of arthrosis in post-menopausal women, with the radiological prevalence of rhizarthrosis in this group of the population at 33% for patients with an average age of 64 years. Of this 33%, only one third of patients present with pain at the base of the thumb. The incidence of rhizarthrosis in males is less than in women (ratio of men to women = 1:10), and it tends to be diagnosed at around 50 years of age. Thus, rhizarthrosis is a process that fundamentally affects post-menopausal women, and it is currently considered as the arthrosis of the upper limbs that leads to the highest number of surgical interventions.
In time, the degeneration of the joint produces flexion of the metacarpal bone, which brings about forced hyperextension of the first phalange and flexion of the second phalange, establishing a Z or M deformity of the thumb. This exacerbates the problem, and the deformity spreads to the other joints, making it difficult to resolve.

Together with the thumb, the trapeziometacarpal joint forms an osteoarticular structure whose physiology and biomechanical pattern need to be known in order to assess the extent of arthrodesis in this joint. Arthrodesis causes the surfaces of the joint to disappear between the trapezium and the first metacarpal, through the fusion of these two bones.
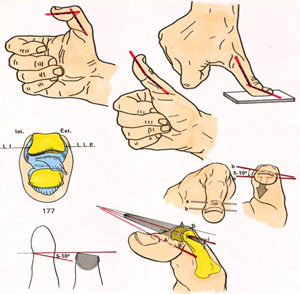
The osteoarticular column offers a high degree of functional flexibility of the thumb, at the expense of the scaphotrapezoid, trapeziometacarpal, metacarpophalangeal and interphalangeal joints. A flexion and extension movement of 50º to 70º is maintained, as is a movement that we could call anterior opposition of 40º to 60º.


The osteoarticular column allows rotation of the axis, which starts at the trapeziometacarpal joint and is accompanied by the metacarpophalangeal and interphalangeal joints. The trapeziometacarpal joint also permits rotation on its longitudinal axis and turning on its transversal axes.
As regards the opposition of the thumb, the trapeziometacarpal and metacarpophalangeal joints are responsible for the anterior position of the thumb, which. Together with the interphalangeal joint, are also responsible for flexion. The movement known as pronation involves the trapeziometacarpal joint; approximately 24º of the movement corresponds to the metacarpophalangeal joint and 7º corresponds to the interphalangeal joint.
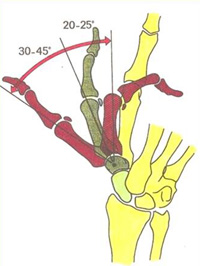
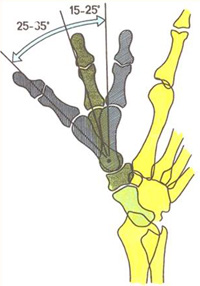
Bearing these biomechanics in mind, we can assert that the fusion of the trapeziometacarpal joint makes the correct opposition possible, since any limitation that might arise is totally offset by the other joints that make up the thumb, provided that the arthrodesis is performed at an abduction angle of 30º-40º, an anterior position of 30º in the 1st metacarpal in relation to the 2nd metacarpal.




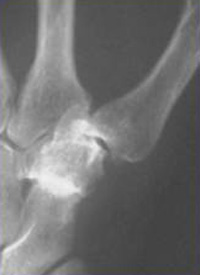
If we wanted to establish a simple classification for rhizarthrosis, we could divide it into 4 types, involving lesser to greater damage to the joint:
- TYPE I: Persistent synovitis, minimal arthrosis and instability of the joint.

- TYPE II: Slight to moderate pinching of the joint, with osteophytes between the metacarpals, but no instability or crepitation.

- TYPE III: Subchondral sclerosis with marked osteophyte and pinching of the joint or severe instability and significant crepitation.

- TYPE IV: A more intense form of Type III, associated with arthrosis in other joints in the thumb column.
The principal indications for performing arthrodesis of the trapeziometacarpal joint are degeneration of the joint or osteoarthrosis, patients with a pattern of hypermobility of the joints leading to subluxation and chronic dislocation, and degeneration of the joint secondary to fractures of the base of the 1st metacarpal or trapezium. It is also indicated in patients with systemic illnesses such as rheumatoid arthritis.
On this occasion, our aim is to provide a retrospective description of patients diagnosed with rhizarthrosis on whom arthrodesis of the trapeziometacarpal joint was performed in the period from January 2003 to September 2008. The data we collected includes, for each patient, their personal details, occupation, diagnostic methods, surgical technique, progression and the results.
We have taken into account the fact that in this document we are only presenting a description of the first data collected.
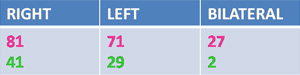
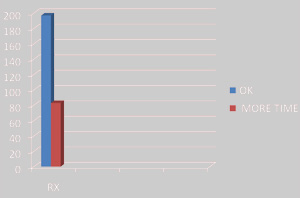
For the period of time in question, 251 patients were diagnosed with rhizarthrosis and 280 trapeziometacarpal arthrodesis procedures were performed, as the procedure was performed bilaterally in 29 cases. The average age was 53.42 years, and patients were monitored for an average period of 3.61 years. In the sample we analysed, 179 cases were in women and 72 cases were in males.

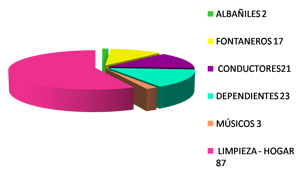
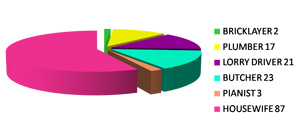
As regards patients’ occupational activities, 153 cases involved a high level of functional demand, and 98 involved a low level of functional demand.
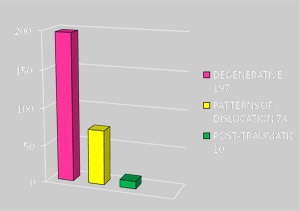
As regards patients’ aetiology, 197 cases were of degenerative origin, 73 cases involved rhizarthrosis secondary to patterns of chronic dislocation and 10 cases involved post-traumatic conditions.


The same diagnostic methods were used in all patients: comparative anteroposterior and lateral x-rays of both hands, and clinical examination for pain, deformity and inflammation at the base of the thumb, irradiating to the entire axis of the index finger and the palm of the hand; loss of strength and limited mobility.
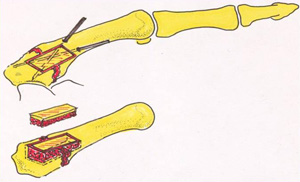
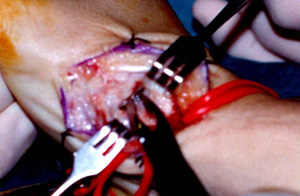
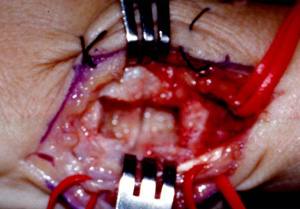
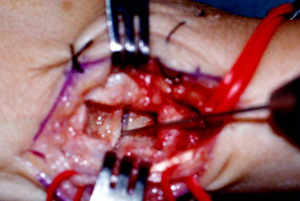
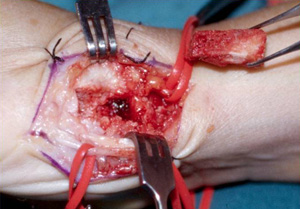
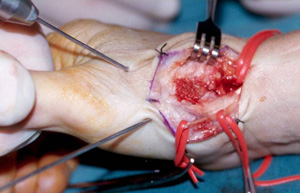
Surgical technique used for arthrodesis of the trapeziometacarpal joint. We used a bone graft of the contralateral iliac crest and osteosynthesis using two cruciate Kirschner needles. It is very important to identify and preserve the sensory branch of the radial nerve. The planes are dissected, the articular capsule is opened up, an arthrotomy is performed and the surfaces of both joints, the trapezium and the metacarpal, are cleaned. A recess is created for the bone graft.
Two Kirschner needles are used for the reduction of the displaced tissue and the fitting of the implant, guided by a fluoroscope in the following position: 30-40º abduction, 30º anterior opposition of the 1st metacarpal in relation to the 2nd metacarpal. The joint is then immobilised using a plaster splint.




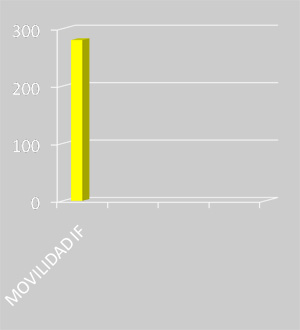
The same post-operative protocol was observed in all patients: after one week, the first post-operative treatment was given and the splint was reapplied. During the 2nd follow-up appointment, 10-15 days after the surgery, the stitches were removed and the final plaster was fitted, to be worn by the patient until consolidation of the bones is confirmed by an x-ray. This tends to occur 50-70 days after the operation, depending on the case. Once that period of time is up, the needles are removed. On certain occasions, and in order to ensure consolidation, after the needles have been removed a plaster splint is left on for 10-20 days, with a view to subsequently starting progressive mobilisation and rehabilitation. After 10-15 sessions, an x-ray is performed and the first functional assessment is carried out. The patients are seen again after a month and a half, four months, six months and one year, and a new functional assessment is carried out at each of these follow-up visits. In the cases we describe here, with an average progression time of 67.4 days, in 197 cases the x-ray was satisfactory and we were able to remove the splint and the Kirschner needles. In 83 cases, the splint was applied for a further 10 to 20 days. The functional assessment at 6 months after the surgery involves assessing the function of the interphalangeal joint, in flexion, active extension and pronation. 100% of our sample had full movement of the interphalangeal joint of the thumb after the surgery. We assessed the function of the metacarpophalangeal joint, which allows flexion at an angle of 60 to 70º, supination at between 5 and 7º and pronation at 20º.
271 patients had full mobility 6 months after the surgery. 9 patients had 35 to 70% mobility; however in all of these patients mobility was completely functional.
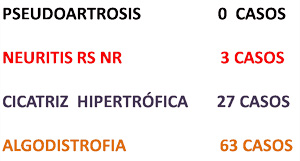
As regards complications, no cases of pseudoarthritis were recorded. There were 3 cases of neuritis of the sensory branch of the radial nerve, which required surgery to release the trapped nerve. There were 27 cases of hypertrophy of the surgical scar, and 63 patients developed Sudeck’s dystrophy, which was resolved in all cases through rehabilitation and calcium and calcitonin supplements.
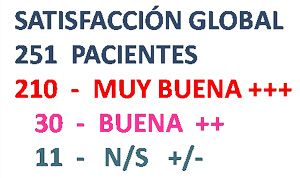
The overall satisfaction of patients was rated as very good++, with highly tolerable levels of residual pain, allowing them to carry out their everyday activities as normal. Only cyclical discomfort was reported, for example with changes in the weather.
Arthrodesis of the trapeziometacarpal joint for the treatment of rhizarthrosis successfully eliminates pain, maintains the functional mobility of the thumb and its strength, and, as such, it is indicated in young patients with a long-term functional demand.
In our experience, we can conclude that arthrodesis of the trapeziometacarpal joint is useful in the treatment of rhizarthrosis. The good medium to long-term results have led us to consider it to be the standard technique in the surgical treatment of rhizarthrosis affecting the trapeziometacarpal joint.





Video:{flv plsize=»0″; height=»350″; width=»400″; img=»/images/stories/LogoAsepeyoVideos2.jpg»}CasoClinicoIII2{/flv}

Video:{flv plsize=»0″; height=»350″; width=»400″; img=»/images/stories/LogoAsepeyoVideos2.jpg»}CasoClinicoIII3{/flv}
Video:{flv plsize=»0″; height=»350″; width=»400″; img=»/images/stories/LogoAsepeyoVideos2.jpg»}CasoClinicoIII4{/flv}
File (spanish) :
Artrodesis trapecio-metacarpiana en el tratamiento de la rizartrosis
La información publicada en este site no reemplaza, sino que complementa, la relación entre el profesional de salud y su paciente o visitante. En caso de duda, consulta con tu profesional de salud de referencia.






